○Jyoji Tanaka, Kazumasa Hoshino
Clinical Implant Society of Japan
Department of Anatomy, Nihon University School of Dentistry at Matsudo
Introduction
Magnetic attachments utilizing magnetic energy, which is an atomic level energy source, have various characteristics that conventional mechanical attachments cannot achieve, and are viewed as effective 3rd generation attachments1,2). A magnetic attachment, however, cannot achieve its full potential if it is used based solely on conventional prosthetic design guidelines because the retention mechanism is completely different from that of mechanical attachments. In previous papers, we highlighted the importance of establishing design guidelines specific to magnetic attachments by classifying them into three groups - Types R, SR and BSR - according to their functional roles 3,4)(Table 1). As a practical approach for clinical application, we have developed a “design chart” based on this functional classification. The chart clearly indicates the prosthetic design guideline to be followed, and simplifies the design process of complete and partial dentures that are stabilized by magnetic attachments, and has proven to be effective for our patients. This presentation reports on the advantages and effectiveness of the chart.
Method
The prosthetic design charts for complete and partial dentures were developed based on the classification of functional roles of magnetic attachments (Table 1), and the effectiveness for clinical application was evaluated. For this study, we used MACS(Magnetic Attachments of a Cap Shape)System, a unique magnetic attachment system consisting of a denture magnet with a pre-mounted resin cap.
Table 1 Classification of magnetic attachments according to functional roles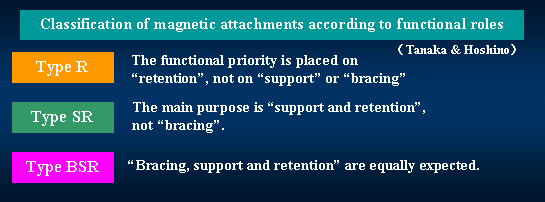
Results
I. Design guideline for complete dentures
Table 2 Design chart for complete dentures (Tanaka & Hoshino)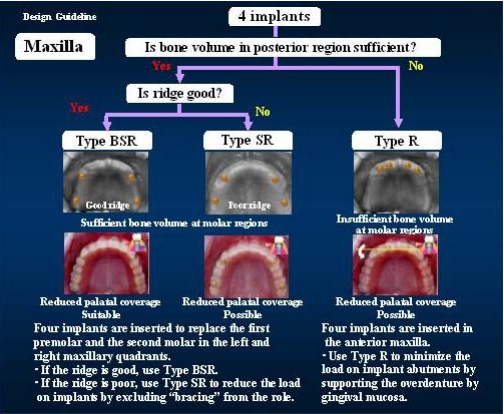
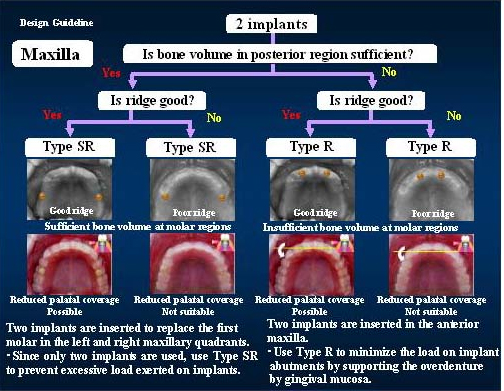
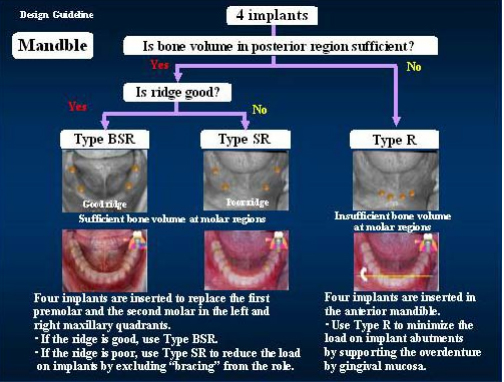
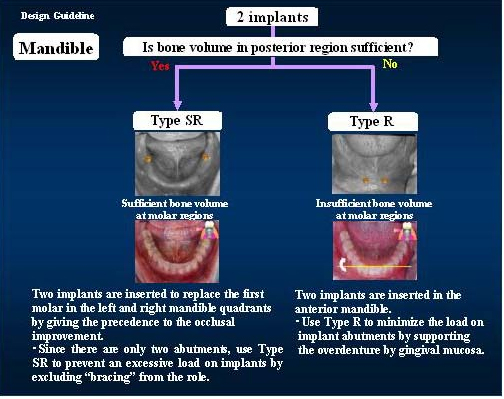

Fig. 1 Two implants are placed to minimize surgical invasiveness. Due to the insufficient bone volume in posterior region, Type R (retention only) is used, as is indicated by the guidelines in the design chart. The purpose of this prosthetic plan is to minimize the load on the two implants placed in anterior region by supporting the overdenture by gingival mucosa.
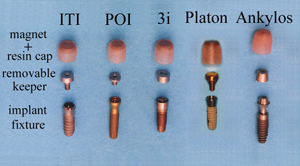
Fig. 2 The MACS System consists of a denture magnet with a resin cap and a removable keeper. Being compatible with various types of implants, the MACS system is structured to simplify the use of magnetic attachments in implant-supported prosthetic restorations. The retentive force of MACS System is approx. 700 gf.
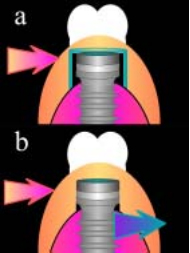
Fig. 3 a) For Type SR and Type R, overdentures are easily fabricated with the MACS System because the system is structured to provide clearance between the keeper and cap to release the lateral force.
b) For Type BSR, there should be no clearance between the keeper and inner surface of the denture to ensure bracing. The MACS System can be used for Type BSR by filling out the clearance with resin after magnet placement.

Fig. 4 In contrast with other attachments, magnetic attachments can cope with implants whose position and/or angle is not optimal. Therefore, implant surgery for magnetic attachments is comparatively easy. The picture above shows a situation in which the removable keepers are placed on the osseointegrated implants.The implants are located to lateral incisor positions in order to enhance the stability of overdenture with only two implants.
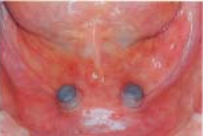
Fig. 5 After re-shaping the margin of resin cap for fine adjustment, connect the denture magnet with the pre-mounted resin cap to the removable keeper, and then take the impression.

Fig. 6 After completion of the master model, fabricate the denture using the standard procedure, and hollow-out the magnet positions on the mucosal aspect of the denture a little deeper in order to make space to accommodate the self-curing resin to attach the magnet.

Fig. 7 Apply a small amount of self-curing resin to the hollowed-out sections, and fit the denture to the magnet in situ. The resin cap can be easily positioned to the hollowed-out section with only a small amount of resin, and there is no need to create a channel to release excessive resin.

Fig. 8 Because the resin cap prevents the self-curing resin from flowing into undercuts, the denture can be left long enough for the resin to cure perfectly without any risk of experiencing difficulties in removing the dentures after polymerization. It should be noted that magnet might slide off if the denture is removed before the resin cures.

Fig. 9 After the resin cures, remove the denture and fill-out the small gap remaining between the margin of the resin cap and the hollowed-out section of the denture. Thus, the magnet overdenture is completed in a simple and easy procedure. Because the MACS System has a space between the resin cap and the keeper, the Type R prosthetic structure can be easily fabricated, and the harmful lateral force from the denture is prevented from being transmitted directly to the fixture.
II. Design guideline for partial dentures
One of the advantages of magnetic attachments is that they make it easy to fabricate combined tooth-/implant-retained restorations. In order to make the best use of this advantage, indications for natural teeth are included in the design guidelines for partial dentures. Eichner classification is used to evaluate missing region and occlusal support in a simple manner(Table 3). Table 4 is the chart for evaluating the functional roles to be provided by attachments.
Table 3 Design chart for partial dentures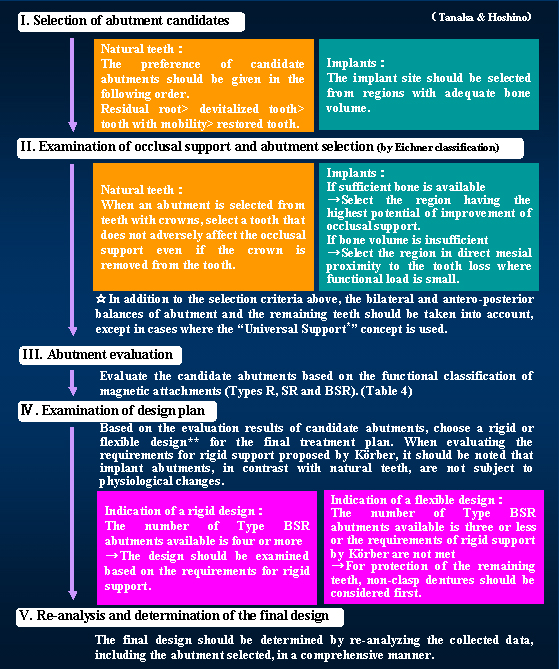
* “Universal Support” refers to a denture design that benefits people of all ages and physical abilities through pursuit of simplicity and ease of use. It also frees patients from feelings of inadequacy because of tooth loss.5,6)(Tanaka & Hoshino)
**The stress-breaking denture design achieved by magnetic attachments is completely different from the conventional “flexible support” concept. To avoid confusion, we define the stress-breaking denture design that uses magnetic attachments as a “flexible design,” and we define the non-stress-breaking denture design that uses magnetic attachments as a “rigid design”.
Table 4 Flowchart for evaluation/judgment of functional role of abutments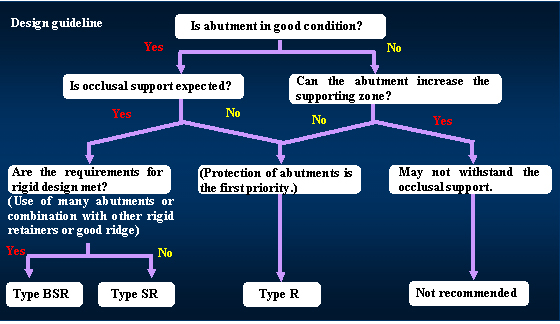
Discussion
I. Design chart for complete dentures
The design chart allowed us to clearly evaluate the factors vital to the design of complete dentures using magnetic attachments, including the number of implants to be inserted, implant positions7,8) and the type of the dentures, which are often determined by the ridge condition, and the functional role to be provided by magnetic attachments. For clinical application, the MACS System was proven to be effective in actually fabricating the dentures based on the design chart due to the ease of modification to suit to the functional role that the attachment should provide.
II. Design chart for partial dentures
The design chart for partial dentures is highly useful because it enables one to make the best use of the advantage of magnetic attachments - ease of combination of tooth-/implant-retained dentures- and allows clear evaluation of factors determining occlusal support that is important in prosthetic design for partially edentulous cases. Through the combined use of Eichner classification and the functional classification of magnetic attachments (Types R, SR and BSR), factors vital to the design of dentures such as the evaluation of occlusal support, the conditions of potential abutments, and the determination of the positions and number of abutment teeth are precisely but easily carried out, thus simplifying the design process of partial dentures stabilized by magnetic attachments. In particular, the use of implants for partial dentures has not been popular due to the difficulties in prosthetic design and handling of retainers. The simple design process provided by the design chart will encourage the use of implants for partial dentures.
Magnetic attachments have been viewed as an excellent retainer and their use is certain to grow in the future. However, definite prosthetic design guidelines for magnetic attachments have yet to be established. For retainers other than magnetic attachments, “bracing” is indispensable in order for them to exhibit retentive force, and it is impossible to prevent the harmful lateral force exerted on dentures from being transmitted to the retainer. Accordingly, denture design using such retainers requires dynamic considerations of abutment teeth and minimization of denture movements as the important factors.
Magnetic attachment, on the other hand, has a unique characteristic in that it can “provide retentive force without bracing,” and the movement of dentures is not directly transmitted to the abutment teeth. The conventional prosthetic design concept contains no consideration to this advantage specific to magnetic attachments.
The design chart we proposed has been developed based on the functional classification of magnetic attachments, and is highly effective in making the best use of the unique advantage of “providing retentive force without bracing.”
Conclusion
The design chart for complete and partial dentures based on the classification of the functional roles of the magnetic attachments has been proven to be highly effective in making the best use of the unique characteristics of magnetic attachments while simplifying the process of prosthetic design.
Aknowledgement
The authors thank the members of MACS Implant Center for their assistances and cooperation in this study.
References
1) Tanaka T. (1992) Magnetic attachments Ver.1. pp. 18-20, 29-39. Tokyo: Ishiyaku Publishers. Inc.
2) Ai M, Mizutani H, Ishihata N, & Nakamura K. (1994) Partial dentures using magnetic attachments. pp. 28-42. Tokyo: Quintessence Publishing.
3) Tanaka J, Hoshino K, Torii S, Furuichi Y, Kashiwabara T, Kakumoto Y, Sato T & Kozawa Y. (2001) Application of Magnetic Attachments for Implants-Part 4. Classification of Magnetic Attachments by the Purpose of Application-. Journal of Japanese Society of Oral Implantology. 14(2) pp. 313-321.
4) Tanaka, J. (2002) Overdenture on osseointegrated implants: State-of-art of implant upperstractures-Part 3. Supplement of QDT. pp. 83-94
5) Ronald M. (1988) Universal Design. Housing for the Lifespan of All People.Washington. D4C,U4S4 Department of Housing and Urban Development.
6) Tanaka J, Hoshino K. (2002) Esthetic prosthesis using magnetic attachments for edentulous patients. Journal of Japan Academy of Esthetic Dentistry. 14(2) pp. 196-203.
7) Zitzmann NU, Marinello CP. (1999) Treatment plan for restoring the edentulous maxilla with implant-supported restorations : removable overdenture versus fixed partial denture design. J Prosthet Dent. 82(2) pp. 188-196.
8) Mericske-Stern RD, Taylor TD, Belser U. (2000) Management of the edentulous patient. Clin Oral Implants Res. (11) pp. 108-25.